TL;DR:
- Lupus erythematosus is an autoimmune disease affecting multiple organs (skin, joints, kidneys). Predominantly affects women aged 16-55 (8x more than men). Incidence: 3-5 per 10,000 people.
- Symptoms: Include fatigue, weight loss, fever, joint pain, skin rash (butterfly erythema), hair loss, muscle pain, heart issues, anemia, cognitive dysfunction, and organ-specific issues (lungs, digestive system, eyes, etc.). May cause osteoporosis.
- Risk Factors: Unknown cause, but associated with genetics, infections, sunlight, hormones, chemicals, high-fat diet, and smoking.
- Diagnosis: Blood tests (antibodies, ESR, CRP), kidney/liver assessment, and imaging studies.
- Treatment: Aim is remission via customized regimens. Universal guidelines: avoid sun, stay active, reduce stress, eat healthy, quit smoking, and use sun protection. Lifelong medical supervision is essential.
- Pregnant women should consult specialists; psychological support is advised.
Autoimmune diseases are a group of conditions in the course of which the immune system attacks its own body. Among such ailments, one of the most serious is lupus. What is this disease, how does it manifest itself and how to treat systemic lupus erythematosus? Find out when you should go to the doctor. Untreated lupus will progress and, in its advanced stage, can be life-threatening.
Lupus – what is it?
Lupus erythematosus is classified as a so-called collagenosis and is one of the systemic connective tissue diseases of an autoimmune nature. The condition is often referred to as "systemic" because it involves multiple organs and tissues, most notably the skin, joints and kidneys and usually other systems as well. Lupus erythematosus occurs predominantly in women (8 times more often than in men) between the ages of 16 and 55. The incidence remains at 3-5 people per 10,000.

Systemic lupus – symptoms
The first symptoms of lupus are primarily:
- weight loss and lack of appetite,
- fatigue,
- enlarged lymph nodes,
- elevated body temperature,
- discomfort in the joints,
- changes in external appearance.
Neurological symptoms, including pain and dizziness, are also characteristic in a disease such as lupus. Lupus can proceed with periods of intensification of symptoms, as well as their withdrawal. One can also distinguish phenomena specific to specific systems and organs that occur in a condition such as systemic lupus. These symptoms usually occur in the area:
- joints – the disease mainly attacks the joints of the wrist, fingers, toes or knees. This is accompanied by swelling pain and sometimes exudation. The symptom is migratory in nature. Pain in one joint that lasts too long can lead to infection of the joint and even bone necrosis,
- skin and mucous membranes – a butterfly-like erythema can be seen on the face, neck and décolleté, but erosions of the mucous membranes of the nose and mouth are also present, and in the later stages of the disease, rim-shaped skin lesions with clear translucency in the center or papules appear. These can occur on the trunk, arms or thighs. In addition, patients may develop pruritus, urticaria or Raynaud's sign. Symptoms of lupus erythematosus sometimes also include thinning and hair loss,
- muscles – wandering muscle pain of varying severity is typical. In the advanced stage, impairment of physical performance and muscle atrophy may occur,
- heart – Libman-Sacks endocarditis and thickening on the heart valves are typical. People with lupus have a much higher risk of atherosclerosis and heart attack,
- blood vessels – inflammation of the walls of veins and arteries can occur,
- lungs – sometimes lung fibrosis, inflammation and lung shrinkage occur,
- nervous system – cognitive dysfunction, mood, anxiety disorders, as well as paresis, seizures, sensory problems, psychosis,
- blood – anemia, reduced platelet and white blood cell count,
- digestive system – abdominal pain, heartburn, ulcers, bleeding, inflammation, vomiting, diarrhea,
- eyes – dry eye, visual disturbances,
- serous membranes – inflammation of the membrane surrounding the lungs, peritonitis, vomiting.
In addition, many diseases can develop just by lupus. The symptoms of osteoporosis may be one of the symptoms of just this autoimmune disorder.
Factors that increase the risk of developing systemic lupus – causes.
The specific cause of lupus is not known. People with genetic predisposition and cases of the disease in the family are at highest risk. However, factors can be listed that increase the risk of developing the condition. These include such as:
- infection with retroviruses or bacteria,
- exposure to sunlight,
- hormonal factors,
- contact with chemicals, especially solvents, aromatic amines and silicon compounds
- taking certain medications.
One factor is also high-fat diet and smoking.
Systemic lupus erythematosus – diagnosis
In the treatment of lupus, it is crucial to diagnose the condition as soon as possible. To this end, upon noticing the first symptoms, it is necessary to see a specialist, such as. dermatologist, rheumatologist or immunologist.  The diagnosis of lupus is made on the basis of tests detecting, among others, antinuclear antibodies, antiphospholipid antibodies, ESR, CRP, syphilis reaction, blood count, assessment of kidney and liver function, coagulation indices or imaging studies.
The diagnosis of lupus is made on the basis of tests detecting, among others, antinuclear antibodies, antiphospholipid antibodies, ESR, CRP, syphilis reaction, blood count, assessment of kidney and liver function, coagulation indices or imaging studies.
Lupus – treatment and specificity of activities
Treatment of lupus is aimed at getting the disease into remission as quickly as possible. Activities and preparations are tailored to the symptoms of the individual patient and focus on the areas and complaints related to the organs that lupus has attacked. 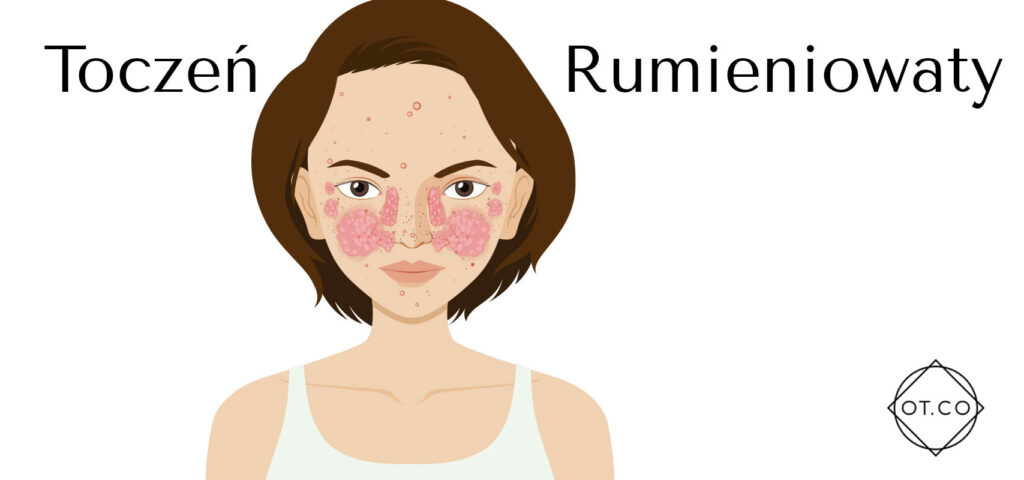 However, it is possible to distinguish general principles used in the treatment of all patients with systemic lupus erythematosus. These are primarily:
However, it is possible to distinguish general principles used in the treatment of all patients with systemic lupus erythematosus. These are primarily:
- avoidance of strong sun exposure and use of appropriate sun protection,
- moderate and regular physical activity,
- rest and avoidance of stress,
- following a healthy diet and quitting smoking,
- use of immunizations and strict adherence to personal hygiene.
It is very important that people with systemic lupus erythematosus remain under the close medical care of their treating physician, as well as specialists who deal with specific organs and systems. For example, joint problems are worth consulting with a rheumatologist, and lupus on the face with a good dermatologist. Specialists for the treatment of lupus and comorbidities can be found at the OT.CO Clinic.
In addition, women planning pregnancy should inform their doctor, who will change the medications they are taking to those that are safe for the baby or temporarily change the form of lupus treatment. It is also recommended to take psychological support. Lupus erythematosus is a disease with which anxiety about the future and fear of advanced and multi-organ ailments are inextricably linked. Such help will also be useful for the patient's loved ones.
Conclusion
Lupus is a complex, systemic autoimmune disease that demands early diagnosis and care. It can affect many organs, causing symptoms like joint pain, skin issues, or severe organ damage. While the exact cause isn’t clear, genetic and environmental factors play a role. Managing lupus requires medical oversight, lifestyle changes, and specialized treatment to ease symptoms and prevent complications. By staying proactive with care, using preventative measures, and consulting specialists as needed, life with lupus can still be lived well. Always prioritize your health and seek medical advice when symptoms appear.