TL;DR:
- Endometrium Overview: The mucous membrane lining the uterine cavity changes with the menstrual cycle, crucial for implantation and pregnancy. Endometriosis occurs when it moves outside the uterus.
- Structure: Composed of epithelial cells, connective tissue, blood vessels, nerves, glands, and immune cells. Divided into the basal (constant) and functional (variable) layers.
- Thickness: Varies by age/cycle (0.3-15 mm). Over 12 mm may indicate endometrial cancer.
- Endometrial Cycle Phases: Multiplication, secretion, exfoliation, driven by hormones (estrogen/progesterone).
- Post-Fertilization: Changes into the gestational membrane for fetal nourishment and immunity.
- Diagnosis Methods: Ultrasound, biopsy, hysteroscopy, curettage.
- Common Diseases: Endometriosis, inflammation, adhesions, polyps, hyperplasia, atrophy, cancer.
- Fertility Issues: 50% of infertile women may have endometriosis, causing tubal obstruction and ovulation issues. Prompt diagnosis is vital for treatment.
The Endometrium is a form of mucous membrane that naturally lining the uterine cavity. It can take on different thicknesses depending on a woman's age and menstrual cycle. During the monthly bleeding cycle, it is the endometrium that regularly exfoliates. Proper work, in turn, affects the ability of the egg to implant after fertilization, as well as the normal course of pregnancy. Sometimes the endometrium also moves outside the uterine cavity. This condition is called endometriosis.
How is the endometrium constructed?
The uterine wall is made up of three layers, consisting of:
- The peritoneal layer that covers the entire organ from the outside,
- Muscular layer, which is the thickest layer that allows the uterine contraction activity,
- The mucous layer located on the inside of the uterus – the endometrium.
endometrial structure The endometrium is built similarly to other mucous membranes. It is made up of epithelial cells, connective tissue and blood vessels, nerves and immune cells. Glands also play a very important role in the structure of the endometrium. Its functions, however, depend on the division of the endometrium into two layers:
- The basal layer located very deep. It is distinguished by its constant structure, which does not depend on the phase of a woman's monthly cycle,
- The functional layer undergoing systematic exfoliation and growth. Such changes in the structure of the endometrium allow the embryo to implant in the uterine wall.
The endometrium changes with each day of a woman's menstrual cycle and age. Changes in the thickness of the endometrium can be seen during an ultrasound examination. Girls who have not yet menstruated should have an endometrium 0.3 – 0.5 mm thick. Mature women, on the other hand, may have an endometrium 7 – 9 mm thick in the first phase of the cycle, and up to 15 mm in the following phases. Women going through menopause, or those on hormone therapy, should in turn have an endometrium of 8 mm thick. When the doctor finds that the thickness of the endometrium exceeds 12 mm during the ultrasound examination, diagnostics for endometrial cancer (uterine cancer) should be performed as soon as possible.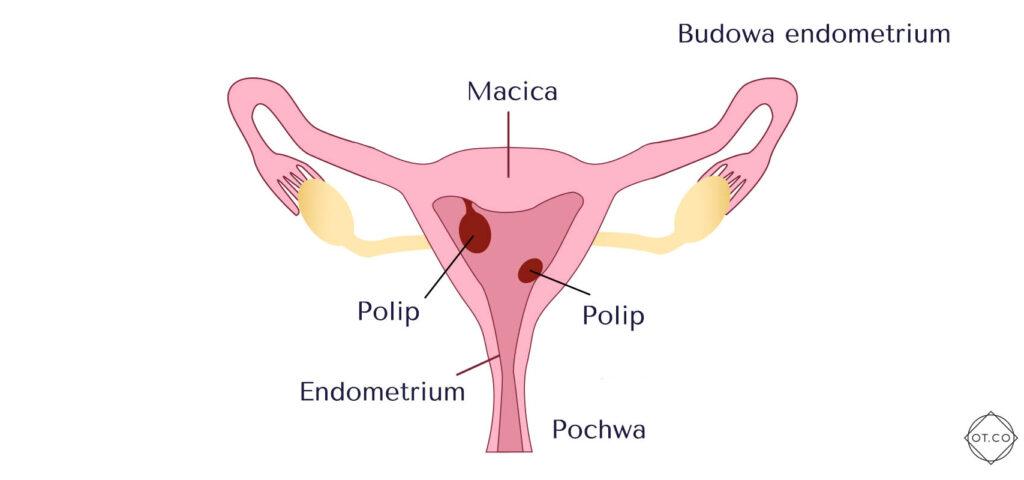
What does the endometrial cycle consist of?
The thickness of the endometrium depends mainly on the concentration of female sex hormones, namely estrogen and progesterone. The behavior of their amount affects the structure of the endometrium on a given day of the cycle. The endometrium is formed by two layers – basal and functional. They are visible during the luteal phase – between ovulation and menstruation. During it, the functional layer slowly peels off, causing menstruation. In the next stage, the functional layer gradually rebuilds from the basal layer. This is made possible by estrogen, which is intensively produced after the 5th day after the onset of menstruation. About halfway through the cycle, or on the 14th day, ovulation occurs. The ovarian follicle releases an egg cell to then change into the corpus luteum, which is responsible for producing progesterone. This hormone, in turn, causes the thickness of the endometrium to increase, and the endometrium becomes ready to receive the embryo. Among other things, the endometrium stores nutrients. When fertilization does not occur, the functional layer undergoes renewed exfoliation, causing menstrual bleeding. Such changes are called the endometrial cycle. It is formed by three phases:
- Multiplication,
- Secretion,
- Exfoliation.
How does the endometrium change after fertilization?
After fertilization of the egg, the endometrium changes its function. Progesterone, which is released from the corpus luteum, causes the membrane to develop and change into the gestational membrane, which is the maternal part of the placenta. It is responsible for the constant flow of blood and nutrients that enable the proper development of the fetus. The temporal layer of the endometrium is formed by a compact and spongy layer. The endometrial tissue is filled with nutrients that guarantee the nesting embryo nourishment until complete implantation. The endometrial tissue also plays an immune role to maintain and carry a pregnancy. This is made possible by immune cells that cause the woman's body to not recognize the fetus as foreign.
What is the diagnosis of endometrial disorders?
Endometrial examinations are usually performed by a gynecologist, who takes a thorough medical history and transvaginal ultrasound during the visit. This test allows verification of the thickness of the endometrium. The ultrasound results are always analyzed on the basis of the medical history and other tests. When the doctor checks during the examination that the endometrium is outside the uterine cavity, then this indicates one of the more common conditions – endometriosis. Endometriosis – causes, symptoms, treatment of endometriosis. Endometriosis is a condition that involves the movement of the endometrium outside the uterine cavity. It can be located in other organs, and menstrual bleeding and peeling of the endometrium causes severe pain for the woman. Endometriosis is also one of the most common causes of infertility in women. Once endometriosis is diagnosed, the specialist offers the woman appropriate treatment. When during the ultrasound examination of the endometrium, the doctor finds the presence of pathological changes, such as polyps, then he refers the patient for further examinations and diagnostics. Other tests involving endometrial diagnosis include:
- Endometrial biopsy which involves taking a piece of endometrial tissue with a special speculum. It is then subjected to microscopic examination. The indication for this examination is mainly for menstrual disorders, bleeding from the reproductive tract, problems getting pregnant and suspected cancer. A sample for examination is also taken during a uterine cavity curettage. It is usually carried out under general anesthesia. During the procedure, the doctor scrapes the endometrium. The curettage allows a larger sample to be taken and gives a good chance of diagnosing the disease.
- Hysteroscopy, a surgical procedure during which a camera is inserted into the uterine cavity to view the endometrium in detail. This allows all pathological changes, such as adhesions, to be seen. The use of the camera means that material for endometrial biopsy is taken from specific areas that look inappropriate to the doctor. Endometrial polyps can also be removed during hysteroscopy.
What are the most common endometrial diseases?
Diseases of the endometrium very often manifest themselves in menstrual disorders, bleeding from the reproductive tract, infertility or complaints of pain. The most common endometrial diseases include:
- Inflammation of the endometrium, which usually occurs after gynecological surgery – cesarean section or uterine curettage. Symptoms associated with this condition include lower abdominal pain, fever and bleeding from the reproductive tract. Bacteria are usually responsible for endometritis, so it is treated with antibiotics.
- Endometrial adhesions taking the form of scarring in the uterine cavity area. Endometrial adhesions can also result from surgery and inflammation. Sometimes they are the cause of problems with getting pregnant and maintaining a pregnancy. The result of adhesions is also Asherman's syndrome, leading to complete overgrowth of the uterus. The initial symptom of adhesions is the disappearance of menstruation and scanty bleeding.
- Polyps of the endometrium in the form of stitched structures. They arise from the proliferated mucosa of the uterus. Polyps are usually not dangerous to health, but always undergo histopathological examination after removal of the lesion. Sometimes cancer cells can be found in their area. Polyps are lesions that are usually no larger than a few centimeters. They do not cause any symptoms, except abnormal bleeding. The lesions can be seen during an ultrasound or hysteroscopy.
- Proliferation of the endometrium involving excessive growth and proliferation of glandular cells. As a result, the endometrium is hypertrophied and too thick. This condition can effectively hinder a woman's ability to function comfortably, as it causes heavy bleeding, including between periods. Proliferation of the endometrium is caused by excess estrogen, and occurs when the thickness exceeds 5 mm in postmenopausal ladies and 8 mm in women taking hormone replacement therapy. The condition usually affects obese women, those using estrogen-containing drugs and those with conditions that cause an increase in estrogen levels.
- Endometrial cancer, the second most common cancer of the female reproductive system. It is usually diagnosed in ladies between about 50 and 70 years of age. The risk of the disease is increased by hormonal disorders, obesity during the menopausal period. Early symptoms indicative of endometrial cancer include abnormal bleeding. Treatment, on the other hand, usually involves surgery and hormone therapy, chemotherapy and radiation therapy are usually complementary treatments.
- Endometriosis involving the displacement of endometrial tissue outside the uterus. This disease can cause pain, infertility and uncomfortable sensations during intercourse. Treatment depends on the severity of the disease and the patient's age. However, therapy is usually based on the administration of hormones or surgical removal of the lesions.
- Endometrial atrophy, a condition in which the endometrium becomes thin due to atrophy of its cells. Endometrial atrophy is caused by a lack of stimulation of the endometrium by estrogen. This phenomenon often occurs during menopause. In women of working age, however, atrophy prevents the embryo from implanting in the uterine wall, leading to secondary infertility.
Gynecological diseases – causes, symptoms and treatments.
Do abnormalities in the endometrium affect fertility?
Problems with getting pregnant are often one of the symptoms of endometriosis. According to studies, even 50% of women struggling with infertility, suffer from endometriosis. Timing plays a big role in treating this condition, as the longer it remains undiagnosed, it reduces a woman's chance of motherhood. Outbreaks of endometriosis cause, among other things, obstruction of the fallopian tubes and damage to the structure of the fallopian tubes. Ovulation disorders and problems with egg fertilization are also common. Some of the tests also detect the adverse effects of the peritoneal fluid of women struggling with endometriosis on sperm motility. This, too, can hinder the fertilization of an egg.
Conclusion
The endometrium plays a vital role in fertility, menstruation, and overall uterine health. It adapts during each menstrual cycle and pregnancy, impacting embryo implantation and pregnancy progression. However, conditions like endometriosis, polyps, and endometrial cancer can disrupt its function, leading to pain, abnormal bleeding, or infertility. Understanding these changes and seeking early medical evaluation for symptoms is crucial for timely treatment. Proper care of the endometrium ensures better reproductive health and prevents complications. Staying informed empowers women to maintain their well-being and make informed health decisions.